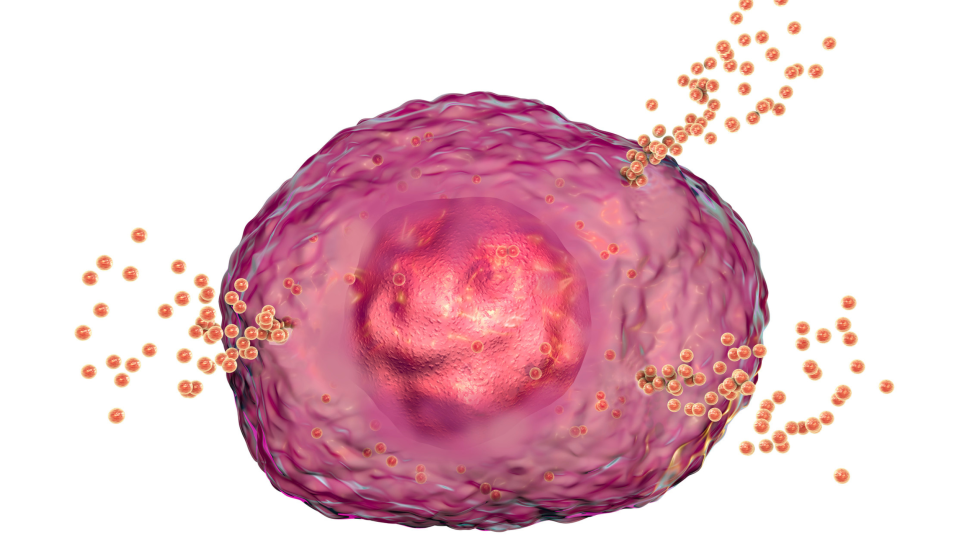
The intricate interactions within our body’s immune system, particularly involving mast cells, play a crucial role in inflammation and allergic reactions. These cells, when triggered by external substances (antigens), can cause inflammation and produce various chemicals that lead to allergic symptoms. Central to this process is a protein called spleen tyrosine kinase (Syk), which, when activated, kicks off a chain reaction leading to these allergic responses.
These allergic responses are responsible for the notorious histamine intolerance many of my patients are afflicted with. I discuss this further in this blog.
However, our bodies have built-in mechanisms to keep this response in check. Another protein, SHP-1, works against Syk to prevent it from going overboard. Interestingly, certain enzymes activated by immune responses can temporarily block SHP-1, intensifying the allergic reaction.
Research highlights several ways to counteract these reactions and stabilize mast cells:
- AMPK Activation: A substance called AMPK can tone down the activation of Syk, helping to control allergic reactions.
- Cyclic GMP: This molecule can activate SHP-1, thereby dampening the allergic response.
- Hydrogen Sulfide (H2S): This gas has a calming effect on mast cells, partly by enhancing the actions of AMPK and cyclic GMP, and also by activating protective cellular defenses.
- Phycocyanobilin (PCB): Found in spirulina, PCB can inhibit certain enzymes involved in allergic responses, showcasing spirulina’s anti-allergic benefits.
- Nutraceuticals: Certain dietary supplements can activate AMPK, increase cyclic GMP levels in mast cells, or enhance the body’s production of H2S, all contributing to reduced allergic reactions.
- Green Tea Catechins: Components found in a specific type of green tea can prevent mast cells from being overly sensitive to allergens.
Understanding these mechanisms offers new avenues for managing allergies and inflammation through diet, supplements, and potentially new treatments, making it easier for individuals to control their allergic responses.
Contemporary Insights into Mast Cell Functions
Mast cells, often linked to allergies, play a broader role in health and disease than previously recognized. Their influence spans across various bodily systems, including the respiratory, neurological, digestive, cardiovascular, skin, uro-genital and musculoskeletal systems. Beyond contributing to allergies, mast cells are involved in infections, cancer, and cardiovascular diseases, showcasing their multifaceted role in both health and disease.
Mast cells possess a wide array of receptors on their surface that detect a multitude of signals, allowing them to respond to different stimuli. The most well-known receptor is the FcεRI, which is primarily activated by antibodies (IgE) and leads to mast cell degranulation. Another receptor, MRGPRX2, is sensitive to various peptides and small proteins, which can trigger allergic reactions, pain, and itching. Mast cells can also react to drugs, cytokines, and physical changes, demonstrating their sensitivity to both internal and external environments.
Upon activation, mast cells can release their stored mediators through three main mechanisms. The first involves the rapid release of pre-formed substances like histamine and heparin through exocytosis. The second phase includes the production and release of newly synthesized molecules such as cytokines and growth factors, independent of the initial degranulation. Lastly, mast cells can release extracellular vesicles like exosomes, which carry proteins, enzymes, and nucleic acids, further influencing the surrounding tissues.
This complexity of mast cell functions underscores their significant impact on various health disorders beyond allergies, highlighting their role in immune regulation and interaction with the environment.
Mast Cell Activation and Release Mechanisms
Mast cells can switch between moving around and releasing their contents, a choice influenced by their internal structure. A key player in rearranging this structure for secretion is mDia1, which helps mast cells move and release substances. Once a mast cell reaches the right spot and detects a trigger, it can release its cargo in several ways: fully merging with the outer cell membrane to release everything, partially merging to form a channel for release, or briefly touching the membrane to release some contents—a method known as “kiss-and-run.” A more subtle release method, observed under electron microscopes, involves small parts of the granules pinching off and fusing with the outer membrane to release their contents. These various release methods influence how quickly and strongly the mast cells react, affecting the body’s response to different stimuli.

Decoding the FcεRI Receptor’s Role in Mast Cell Activation
The FcεRI receptor is crucial for triggering mast cell degranulation and the surge in pro-inflammatory lipids and cytokines. This receptor, a complex structure, binds tightly to IgE present outside the cell.
When IgE binds to specific antigens, it triggers FcεRI receptor complexes to cluster together. This clustering activates Lyn, a src-family tyrosine kinase, which then phosphorylates the γ subunit of the FcεRI complex. This action allows spleen tyrosine kinase (Syk) to attach and become activated by Lyn. Activated Syk then modifies the LAT protein, attracting various proteins to assemble a signaling complex. This complex activates downstream enzymes and kinases such as phospholipase C-γ, PI3K, and NADPH oxidase, leading to a cascade of immune responses.
These molecules work in concert to kickstart mast cell degranulation and ramp up the production of inflammatory cytokines and lipid mediators. Though Fyn, another src-family kinase, can step in for Lyn in some roles, Syk’s activation is pivotal for mast cell response, underscoring its central importance in the signaling pathway.
Balancing Mast Cell Activation: The Role of Tyrosine Phosphatases
Mast cell activation is a complex process involving a delicate balance between tyrosine kinase signaling, which promotes activation, and the opposing force of tyrosine phosphatases, which temper this response. Central to this balancing act is the Src homology region 2 domain-containing phosphatase 1 (SHP-1). SHP-1 plays a crucial role in mast cells by counteracting the signaling initiated by the FcεRI receptor upon antigen detection. It does this by reversing the phosphorylation of key proteins, such as LAT and SLP-76, which are phosphorylated by Syk as part of the mast cell activation process.
Hydrogen Peroxide
However, the activity of SHP-1, and tyrosine phosphatases in general, is vulnerable to physiological concentrations of hydrogen peroxide. This oxidant can inhibit SHP-1 by modifying its cysteine residues, essentially up-regulating the tyrosine kinase signaling pathway indirectly. This mechanism is part of how oxidants can amplify signaling pathways, leading to increased mast cell activation.
Hydrogen peroxide (H2O2) is a reactive oxygen species (ROS) produced naturally within the body. It plays crucial roles in signaling pathways, immune responses, and cellular homeostasis. The main sources of hydrogen peroxide in the body include:
- Mitochondrial Respiration: The mitochondria are known as the powerhouse of the cell, where oxygen is used to produce energy in the form of ATP. A small percentage of the oxygen consumed by the mitochondria undergoes incomplete reduction, leading to the formation of superoxide radicals, which are then converted into hydrogen peroxide by the enzyme superoxide dismutase (SOD).
- Enzymatic Production: Several enzymes in the body produce hydrogen peroxide as a byproduct. These include amino acid oxidases, urate oxidase, and xanthine oxidase, among others. For example, during the breakdown of certain amino acids, amino acid oxidases can produce hydrogen peroxide.
- NADPH Oxidase: This enzyme complex, found in the membranes of phagocytes like neutrophils and macrophages, generates superoxide radicals by transferring electrons from NADPH inside the cell to oxygen molecules outside the cell. The superoxide radicals are then rapidly converted into hydrogen peroxide, which is used by the immune system to kill invading pathogens.
- Peroxisomes: These are organelles that contain oxidative enzymes, such as catalase and urate oxidase, that produce and break down hydrogen peroxide. Peroxisomes play a key role in lipid metabolism and the detoxification of hydrogen peroxide.
- Cytochrome P450 Enzymes: These enzymes, located in the endoplasmic reticulum of liver cells and other tissues, are involved in the metabolism of various substances, including drugs and toxins. The activity of cytochrome P450 enzymes can lead to the production of hydrogen peroxide.
Hydrogen peroxide acts as a signaling molecule that can modify proteins through oxidation, affecting various biological processes. However, excessive production of hydrogen peroxide can be harmful, leading to oxidative stress and damage to cellular components. The body has antioxidant mechanisms, such as catalase and glutathione peroxidase, to neutralize excess hydrogen peroxide and maintain cellular health.
The production of superoxide, which can convert to hydrogen peroxide near the plasma membrane, seems to play a pivotal role in this process. Its generation early in mast cell activation leads to the suppression of SHP-1, thus favoring the continuation of the activation cascade through Syk-mediated phosphorylations.
Superoxide is a reactive oxygen species (ROS) generated in the body primarily through the following sources:
- Mitochondrial Electron Transport Chain: The most significant source, where superoxide is produced as a byproduct of oxygen metabolism during ATP synthesis.
- NADPH Oxidase: Present in immune cells like neutrophils and macrophages, this enzyme complex produces superoxide to kill pathogens.
- Cytochrome P450 Enzymes: Involved in drug metabolism in the liver, these enzymes can also generate superoxide during the breakdown of various substances.
- Xanthine Oxidase: An enzyme that produces superoxide during purine metabolism, particularly in conditions like ischemia.
- Uncoupling of Nitric Oxide Synthase (NOS): When deprived of its cofactors, NOS can produce superoxide instead of nitric oxide.
While superoxide plays roles in cell signaling and defense against pathogens, excessive production can lead to oxidative stress and cellular damage, necessitating its prompt detoxification by superoxide dismutase (SOD) into less harmful substances like hydrogen peroxide.
Interestingly, the induction of heme oxygenase-1 (HO-1) in mast cells shows promise in opposing mast cell degranulation and overall activation. The bilirubin produced by HO-1 acts as an inhibitor of the NADPH oxidase activity, a source of superoxide, thus providing a potential pathway to mitigate excessive mast cell responses. This highlights a fascinating aspect of cellular regulation where the body’s own mechanisms to generate and quench reactive oxygen species can profoundly influence immune cell behavior.
Boosting Hemoxygenase is Critical. More on that here in this video.
Molecular Pathways to Inhibit Mast Cell Activation
Discoveries in cellular biology have illuminated several pathways that can effectively dampen the activation of mast cells, which are crucial in allergic reactions and inflammation. Key among these are the actions of AMP-activated protein kinase (AMPK), the rise of cyclic GMP (cGMP), and the generation of hydrogen sulfide (H2S). Each of these molecules plays a significant role in regulating mast cell degranulation, the process by which mast cells release their inflammatory contents.
AMPK, a cellular energy sensor, has been observed to interfere with the binding of key enzymes Lyn and Syk to the FcεRI receptor complex on mast cells. This receptor is pivotal in triggering mast cell activation upon encountering an antigen. While the exact mechanism remains to be fully understood, AMPK’s activation results in a modification of the receptor’s beta chain, which might hinder Lyn’s interaction and, as a result, reduce mast cell activation.
Cyclic GMP, another critical regulator, operates through the protein kinase G II (PKGII), which can enhance the activity of SHP-1, a phosphatase that deactivates signaling pathways leading to mast cell degranulation. The potential of cGMP to curb mast cell activation through SHP-1 signifies an intriguing area for further research. Additionally, the enzyme heme oxygenase-1 (HO-1) appears to contribute to this regulatory mechanism by generating carbon monoxide, which then stimulates cGMP production, adding another layer of control over mast cell degranulation.
Understanding these regulatory pathways opens new avenues for developing treatments aimed at controlling allergic reactions and inflammation by targeting these specific mechanisms to prevent excessive mast cell activation
Harnessing Hydrogen Sulfide to Subdue Mast Cell Activation
Recent research has highlighted the potent ability of hydrogen sulfide (H2S) to suppress mast cell degranulation, a pivotal process in allergic reactions and inflammation. H2S can be generated endogenously in the body or delivered through H2S-releasing drugs, offering a promising avenue for therapeutic intervention.
H2S exerts its anti-inflammatory effects through several key mechanisms. Notably, it can activate the AMP-activated protein kinase (AMPK) pathway, which is known to play a role in inhibiting mast cell activation. This activation is facilitated through a cascade involving calcium/calmodulin-dependent kinase kinase-β, which in turn, enhances AMPK activity.
Additionally, H2S contributes to the cellular defense mechanism by inducing the expression of heme oxygenase-1 (HO-1), an enzyme with anti-inflammatory properties. It achieves this by modifying the protein Keap1, thereby preventing it from inhibiting the transcription factor Nrf2. This leads to an increased transcriptional activity of Nrf2, which is responsible for the expression of genes that provide protection against oxidative stress, including HO-1. Many of my patients have mutations in HO-1 as well as HO-2. I describe ways to induce HO-1 below in the recommendations.
Moreover, H2S boosts the production of cyclic GMP (cGMP) within mast cells, both by reversing the oxidative inhibition of soluble guanylate cyclase (sGC) and by inhibiting phosphodiesterase 5 (PDE5), an enzyme that degrades cGMP. The role of cGMP in mast cell regulation is significant, as it is known to suppress degranulation. Supporting this, drugs that inhibit PDE5, such as vardenafil, have been shown to counteract mast cell degranulation effectively.
These findings underscore the potential of H2S and related pathways as targets for novel treatments aimed at controlling allergic reactions and inflammatory conditions by mitigating mast cell activation.
How is Hydrogen Sulfide (H2S) produced?
Hydrogen sulfide (H2S) is produced in the body through the activity of specific enzymes that metabolize sulfur-containing amino acids. The main enzymes responsible for H2S synthesis are:
- Cystathionine β-synthase (CBS): Predominantly found in the brain and liver, CBS uses homocysteine and serine as substrates to produce H2S. This is a common mutation found in many people with mast cell disorders. This is a vitamin B6 dependent enzyme.
- Cystathionine γ-lyase (CSE): This enzyme is primarily active in the cardiovascular system and liver, converting cystathionine into cysteine, which can then be used to generate H2S. This is a common mutation found in many people with mast cell disorders.
- 3-Mercaptopyruvate sulfurtransferase (3-MST): Found in many tissues, including the brain and vascular endothelium, 3-MST generates H2S from 3-mercaptopyruvate, a product of cysteine catabolism.
These enzymes work in various metabolic pathways to produce H2S, which acts as a signaling molecule regulating diverse physiological functions, including vasodilation, neurotransmission, and inflammation modulation.

Increasing hydrogen sulfide (H2S) levels in the body can be achieved through dietary means, supplements, and lifestyle practices that stimulate its endogenous production or provide precursors. Here are several ways to potentially increase H2S levels:
- Dietary Sulfur-rich Foods: Consuming foods high in sulfur, such as garlic, onions, leeks, and cruciferous vegetables (e.g., broccoli, Brussels sprouts, cauliflower), can boost cysteine levels, a precursor for H2S production.
- Amino Acids Supplementation: Supplements containing cysteine, such as N-acetylcysteine (NAC), can provide the necessary substrates for H2S synthesis. Methionine, another sulfur-containing amino acid, can also support H2S production indirectly.
- Increase Taurine Intake: Taurine, found in meat, fish, and dairy, can enhance the expression of enzymes like CBS and CSE, which are involved in H2S production.
- MSM (Methylsulfonylmethane) Supplement: MSM is an organic sulfur compound that might increase sulfur availability in the body, potentially boosting H2S production.
- Alpha-lipoic Acid: This antioxidant can increase the expression of H2S-producing enzymes, thereby potentially raising H2S levels.
- Physical Exercise: Regular exercise can enhance the activity of enzymes like CBS and CSE, increasing H2S production.
- Reduce Oxidative Stress: Minimizing oxidative stress through antioxidants intake (e.g., vitamin C, vitamin E) may preserve the function of H2S-producing enzymes.
- Hydrogen-rich Water: Some research suggests that drinking hydrogen-rich water might indirectly affect H2S levels, though more research is needed in this area.
Remember, while boosting H2S can have health benefits, it’s important to approach any supplementation or significant dietary changes with caution and, if possible, under the guidance of a healthcare professional

Sulfur: Double edged sword
Sulfur intolerance can arise from several factors, including genetic predispositions, gut microbiome imbalances, and environmental exposures. Here’s a closer look at the common causes:
- Genetic Variations: Certain genetic mutations can affect the body’s ability to metabolize sulfur compounds. For example, mutations in the CBS (Cystathionine Beta-Synthase) gene can lead to an increased production of sulfur-containing compounds, potentially resulting in sulfur intolerance.
- Gut Microbiome Imbalance: An imbalance in the gut microbiome can affect the digestion and processing of sulfur-rich foods. An overgrowth of sulfur-reducing bacteria may lead to excessive hydrogen sulfide production, which can cause gastrointestinal symptoms and contribute to sulfur intolerance.
- Impaired Detoxification Pathways: If the body’s detoxification pathways are compromised, processing and eliminating sulfur compounds can be challenging, leading to symptoms of intolerance. This can be due to genetic factors, nutrient deficiencies (such as B vitamins and magnesium), or exposure to toxins that burden the detox system.
- Inadequate Nutrient Levels: Certain nutrients are essential for metabolizing sulfur-containing compounds. Deficiencies in nutrients like molybdenum, B vitamins (especially B6 and B12), and magnesium can impair sulfur metabolism, leading to intolerance symptoms.
- Increased Intake of Sulfur-rich Foods: Consuming a diet high in sulfur-rich foods (like cruciferous vegetables, garlic, onions, and animal proteins) can exacerbate intolerance symptoms in susceptible individuals.
- Environmental Toxins: Exposure to environmental toxins that contain sulfur or disrupt sulfur metabolism can also contribute to intolerance.
- Leaky Gut Syndrome: Increased intestinal permeability (leaky gut) can allow larger sulfur compounds to enter the bloodstream, potentially leading to an intolerance response.
Addressing sulfur intolerance typically involves identifying and mitigating the underlying cause, adjusting the diet to manage sulfur intake, supporting gut health, and enhancing the body’s detoxification capabilities.
Nutraceutical Approaches for Enhancing Mast Cell Stability
The intricate roles mast cells play in allergic reactions present a compelling case for exploring nutraceutical interventions that could potentially stabilize these cells, thus mitigating allergic responses. Here, we delve into various nutraceutical compounds that show promise in this regard, based on their biological mechanisms of action.
Note- many of these are in Vykon, a customized nutritional supplement that all my patients get after they do an HTMA. This is one of the many reasons may of their mast cell and histamine issues resolve when working with out clinic. To learn more about the HTMA and Vykon, visit this page.

A great way to Jump Start your healing is the HTMA Supercharged program.
Berberine: This compound, derived from traditional Chinese medicinal herbs, has garnered attention for its effectiveness in managing type 2 diabetes and lowering lipid levels. Its mode of action is attributed to the activation of AMP-activated protein kinase (AMPK), akin to the diabetes drug metformin. Berberine has demonstrated the capacity to inhibit mast cell degranulation by curtailing Syk phosphorylation, a process expected from an AMPK activator. Animal studies have shown its protective effects in models of allergic rhinitis and anaphylaxis induced by various allergens.
Phase 2 Inducing Agents: These agents, through the Nrf2-mediated induction of heme oxygenase-1 (HO-1), can suppress mast cell NADPH oxidase activity and elevate cGMP levels, contributing to mast cell stabilization. Notable among such agents are lipoic acid and sulforaphane from broccoli sprout extract (BSE), both of which have shown clinical benefits. Lipoic acid has been protective in anaphylaxis models, while BSE has shown to alleviate symptoms of allergic rhinitis and modulate the allergic response to environmental pollutants in clinical studies.
Melatonin: Known for regulating sleep, melatonin also exerts an immunomodulatory effect by increasing Nrf2 expression, thereby promoting phase 2 induction. It enhances AMPK activity indirectly through the induction of Sirt1 and mitigates the NF-kappaB-mediated activation phase of mast cells. Efficacy of melatonin in reducing allergic rhinitis symptoms and suppressing mast cell degranulation under stress has been observed in animal models, along with a reduction in inflammatory cytokine production by mast cells.
Nrf2 Activation’s Role in Mast Cell Stabilization: Emphasizes the significance of Nrf2 activation in countering MRGPRX2 signaling, which is associated with pseudo-allergic mast cell activation, highlighting a new approach to managing allergic responses. Many of my patients have mutations in Nrf2 and an upregulation of Keap1, which inhibits Nrf2 from functioning properly.
Paeoniflorin’s Mast Cell Stabilizing Effects: Details the use of paeoniflorin, from peony flower extracts, as a natural compound with proven effectiveness in stabilizing mast cells across mast cell cultures and animal allergy models, underscoring the need for further investigation into its mechanisms.
Phycocyanobilin (PCB) from Spirulina: Discusses PCB’s mimicking of bilirubin’s inhibitory effects on NADPH oxidase activity. This action contributes to spirulina’s observed antioxidant and anti-inflammatory benefits in rodent models, offering potential for allergic symptom alleviation and mast cell stabilization.
Biotin’s Potential in Mast Cell Activity Modulation: Explores the intriguing potential of high-dose biotin supplementation in activating soluble guanylate cyclase (sGC), suggesting a novel, non-hypotensive method to influence mast cell activity and potentially offering a new therapeutic direction.
N-acetylcysteine (NAC) for H2S Production: Highlights how NAC, by supplying cysteine, can boost the body’s production of hydrogen sulfide (H2S) through enzymes CBS and CSE, offering a pathway to stabilize mast cells and mitigate allergic reactions.
NAC’s Role in Reversing Oxidative Inhibition: Discusses NAC’s secondary benefit of promoting glutathione synthesis, potentially counteracting the oxidative inhibition of SHP-1, a phosphatase that deactivates mast cell activation signals.
Taurine’s Potential Benefits: Explores the evidence supporting taurine’s ability to enhance expression of H2S-producing enzymes in vascular tissues and its potential, though unconfirmed, effects in mast cells, along with its demonstrated efficacy in reducing allergic symptoms in animal models.
Benifuuki Green Tea’s Unique Properties: Details the special characteristics of benifuuki green tea, rich in O-methylated EGCG, which shows superior bioavailability and effectiveness in seasonal allergy management. The potential mechanisms include mast cell stabilization and down-regulation of the FcεRI receptor, offering a promising, albeit underexplored, option for allergy sufferers.
This concise overview outlines natural strategies for mast cell stabilization, spotlighting the roles of NAC, taurine, and benifuuki green tea. Each component offers unique mechanisms for potentially reducing allergic responses and enhancing overall immune balance.
Zeolite, a natural mineral known for its unique cage-like structure, has gained attention for its potential in health and wellness, particularly in detoxification processes and reducing histamine levels in the body.
Inducing HO-1 (esp important for those who have mutations)
Inducing heme oxygenase-1 (HO-1), an enzyme with protective effects against oxidative stress and inflammation, can be achieved through nutritional and nutraceutical interventions. Here are some strategies:
Nutritionally:
- Cruciferous Vegetables: Broccoli, Brussels sprouts, and kale are rich in sulforaphane, a potent inducer of HO-1. Including these vegetables in your diet can boost HO-1 levels.
- Curcumin: Found in turmeric, curcumin is known to induce HO-1 expression. Adding turmeric to meals or drinking turmeric tea can help elevate HO-1.
- Resveratrol: This compound, present in red grapes, peanuts, and berries, has been shown to induce HO-1. Incorporating resveratrol-rich foods into your diet or considering a supplement can be beneficial.
- Green Tea: The catechins in green tea, especially epigallocatechin gallate (EGCG), can induce HO-1. Drinking green tea regularly is an easy way to leverage this effect.
Nutraceutically:
- Sulforaphane Supplements: For those who may not consume enough cruciferous vegetables, sulforaphane supplements are an alternative to induce HO-1.
- Curcumin Supplements: High-quality curcumin supplements, especially those with enhanced bioavailability, can effectively induce HO-1. Look for products containing piperine, which increases absorption.
- Resveratrol Supplements: High-dose resveratrol supplements can induce HO-1. Since dietary sources provide resveratrol in small amounts, supplements might offer a more concentrated dose.
- N-Acetylcysteine (NAC): NAC is a precursor to glutathione, an antioxidant that can indirectly support HO-1 induction by reducing oxidative stress.
- Astaxanthin: This powerful antioxidant, found in algae and the marine animals that eat them, has been shown to induce HO-1 and offers a broad range of health benefits.
- Coffee Extracts: Certain compounds in coffee, not just caffeine, have been associated with the induction of HO-1. Coffee extract supplements could be an alternative for non-coffee drinkers.
When considering the use of any supplements, it’s crucial to consult with a healthcare provider to ensure they’re appropriate for your health status and won’t interact with any medications you’re taking.
The Healing Power of Zeocharge Zeolite
My favorite zeolite for myself and my patients is Zeocharge. You can purchase that here
Use coupon ICHealer for 10% discount.

The mechanism by which zeolite may help in managing histamine levels involves several key actions:
- Absorption of Histamine: Zeolite’s porous structure allows it to act as a molecular sieve, absorbing and trapping various substances, including histamine. By binding to histamine in the gut, zeolite may prevent its absorption into the bloodstream, thereby reducing histamine levels in the body and alleviating related allergic or inflammatory responses.
- Detoxification: Zeolite is known for its detoxifying properties, thanks to its ability to bind heavy metals, toxins, and other harmful substances, facilitating their removal from the body. By reducing the overall toxic burden, zeolite can indirectly support the immune system’s proper functioning, potentially leading to a more regulated and less hyper-reactive response that could otherwise result in excessive histamine release.
- Supporting Gut Health: Given that a significant portion of the immune system is located in the gut, maintaining gut health is crucial for managing histamine levels. Zeolite can support gut health by absorbing harmful substances and promoting a healthy gut environment. This can help reduce gut inflammation and the risk of leaky gut syndrome, conditions associated with increased histamine production and release.
- Antioxidant Properties: Zeolite exhibits antioxidant properties, helping to neutralize free radicals and reduce oxidative stress. Since oxidative stress can trigger and exacerbate inflammation and histamine release, the antioxidant action of zeolite may contribute to lower histamine levels and reduced allergic reactions.
It’s important to note that while zeolite shows potential in managing histamine levels and providing other health benefits, its use should be approached with caution. The quality of zeolite supplements can vary, and not all forms are suitable for consumption. Consulting with a healthcare provider before starting any new supplement regimen, including zeolite, is advisable to ensure safety and appropriateness for your specific health needs.
Conclusion
Concluding our exploration into the power of nutraceuticals for managing allergies and stabilizing mast cells, we’ve uncovered a variety of compounds with potential benefits. Berberine, spirulina (or its component PCB), lipoic acid, broccoli sprouts, melatonin, NAC (N-acetylcysteine), taurine, high-dose biotin, and benifuuki tea catechins collectively offer a promising approach to down-regulate FcεRI signaling, which is pivotal in allergic reactions.
The mechanisms through which these agents exert their effects include enhancing mast cell stability, inhibiting pro-inflammatory signaling, and supporting the body’s natural antioxidant defenses. While further research, particularly in rodent models of allergy, is needed to refine these regimens, the cumulative effect of these interventions suggests a significant potential for clinical benefit in allergy management.
While the suggested dose schedules are based on their demonstrated impact in various health contexts, they provide a starting point for consideration in allergy control strategies. Future studies should aim to optimize these doses specifically for managing allergies, potentially offering those affected a complementary or alternative approach to conventional treatments.
To learn more about how you can investigate your Root Cause, check out the Root Cause Investigation.
References
Mark F McCarty, Aaron Lerner, James J DiNicolantonio & Carina Benzvi (2021) Nutraceutical Aid for Allergies – Strategies for Down-Regulating Mast Cell Degranulation, Journal of Asthma and Allergy, 14:, 1257-1266, DOI: 10.2147/JAA.S332307