[et_pb_section fb_built=”1″ admin_label=”section” _builder_version=”3.22″][et_pb_row admin_label=”row” _builder_version=”4.9.7″ background_size=”initial” background_position=”top_left” background_repeat=”repeat” hover_enabled=”0″ sticky_enabled=”0″][et_pb_column type=”4_4″ _builder_version=”3.25″ custom_padding=”|||” custom_padding__hover=”|||”][et_pb_text admin_label=”Text” _builder_version=”3.27.4″ background_size=”initial” background_position=”top_left” background_repeat=”repeat”]
It is more common than you think!
Oxalate issues are not as simple as “cut out your oxalates and you will heal”. This is a common misconception. From my own personal experience, the low oxalate diet alone did not heal my body. I learned on my own that I had multiple contributors to my oxalate problem, as do many of my patients.
As many people know I often focus on oxalates when it comes to investigating the root cause of IC/BPS.
Here are some of my interviews:
I often am asked why some people are more vulnerable to oxalates than others. There are many factors involved in this, so I want to summarize a few of them. In this blog, I want to focus on Enteric Hyperoxaluria.
Generally, only 10 percent of oxalate from the diet is absorbed in a normal, healthy gut. Absorbing only ten percent from diet doesn’t seem like much — but even in young healthy people — if you consume enough of this stuff, you can damage the intestinal lining and create conditions which deplete antioxidants like glutathione. This in turn, upregulates your endogenous oxalate production due to oxidative stress.
It truly is a web that requires detailed lab testing and analysis to untangle, because every person’s root cause is so different. However, I do think many people are dealing with a form of Enteric Hyperoxaluria.
First, what are oxalates?
Oxalates are a poison, plain and simple. They are ant-nutrients found in plant foods, and highest in foods such as spinach, beets, Swiss chard, and rhubarb. They are also produced by yeast, fungus, and mold. Depending on your genetics, a small quantity is also produced by human metabolism. There are also other factors that can increase your production of oxalates within your metabolism that I will describe shortly. They also chelate minerals such a Ca, Mg, Zinc and iron. A big contributor to this is often Enteric Hyperoxaluria.
Why so much focus on oxalate?
In summary, oxalates have a negative impact on the body through multiple mechanisms. These include mechanical shredding, the increase in free radicals and the decrease in antioxidants. They are associated with multiple varied pathologies impacting a tremendous number of different organs and body systems. They are an independent trigger of the upregulation of the NOX1 enzyme, becoming an independent trigger of mast cell activation syndrome. And they can be caused by multiple environmental causes, multiple dysfunctions in the body and multiple genetic causes, including Enteric Hyperoxaluria.
Oxalates are a poison
They are a poison in the body. And they poison us in several different ways. One of the main ways is that they destroy mitochondrial function through several different mechanisms. They halt ATP synthesis, but they also shred intracellular organelles, including the mitochondria. Additionally, they alter our redox homeostasis. They do this through different mechanisms, including the depletion of glutathione, the depletion of superoxide dismutase, and the depletion of NADPH oxidase. This is a problem because need to reduce glutathione from its oxidized state.
And we do this through the up regulation of a pathway called NOX1, or NADPH oxidase one. The upregulation of NOX is pretty significant because that in turn creates additional superoxide. This is where we see that depletion of superoxide dismutase coming in. Also, many of my patients also have polymorphisms in this enzyme, which complicates this even more. And if we exceed our capacity to convert superoxide into hydrogen peroxide, we develop an independent trigger for mast cell activation syndrome. As such oxalates can be an independent trigger for people who are struggling with mast cell issues. For those with an underlying form of Enteric Hyperoxaluria, this can be a recipe for disaster.
Cellular damage
So once those crystals are deposited into tissue, they mechanically shred that surrounding tissue because it is not an exaggeration to say that they are like little needles or little razor blades or shards of glass in the body.
So because they are so small, nano sized, they are able to enter the cells and they cause progressive harm as they do so.
We see things like:
-
- apoptotic and necrotic cell death
-
- rupture of cell membranes
-
- lysosomal rupture
-
- cell shrinkage, nuclear shrinkage
-
- destruction of intracellular organelles, including but not limited to mitochondria
This is part of the connection that we see between chronic fatigue syndrome and hyperoxaluria, the physical destruction of these mitochondria. Pretty hard to make ATP when you don’t have enough functioning mitochondria. Oxalate is also implicated in breast cancer and autoimmune thyroiditis. This can also be where the cellular damage can really impact certain diseases that do not seem overtly involving oxalate.
The dangers of a high fat diet
The dieting and health industry loves to go to extremes with certain dieting trends. The latest fad is the ketogenic and carnivore diet. I will continue to stand by this, I do not think these diets are health long term. Once you understand how they can worsen oxalate absorption, you will see why I stand so strong by this philosophy.
There was an article published in the Clinical Journal of the American Society of Nephrology. This journal discussed that “enteric hyperoxaluria is a distinct entity that can occur as a result of diverse set of gastrointestinal disorders that promote fat malabsorption. This in turn, lead to excess absorption of dietary oxalate and increased urinary oxalate excretion”. This is huge!

Witting, C., Langman, C. B., Assimos, D., Baum, M. A., Kausz, A., Milliner, D., Tasian, G., Worcester, E., Allain, M., West, M., Knauf, F., & Lieske, J. C. (2021). Pathophysiology and Treatment of Enteric Hyperoxaluria. Clinical journal of the American Society of Nephrology : CJASN, 16(3), 487–495. https://doi.org/10.2215/CJN.08000520
Enteric hyperoxaluria explained
Coming directly from the article
“Oxalate is an end product of glyoxalate metabolism in the liver. The remainder of systemic oxalate comes from ingestion of certain fruits and vegetables. The oxalate in these plants is in the form of relatively insoluble calcium oxalate crystals. Hence, under normal conditions, only 5%–10% of ingested oxalate is absorbed and the remainder passes into the stool. However, in patients with fat malabsorption of any cause (enteric hyperoxaluria), undigested fatty acids reach the large intestine where they can combine with calcium; (B) the net effect is to release more free oxalate into the intestinal lumen. It is thought that this free oxalate is largely absorbed paracellularly in the large intestine. Due to the fat malabsorption, among patients with enteric hyperoxaluria, the net percentage of ingested oxalate that ends up being absorbed can increase to ≥30%. Any oxalate that comes from the liver or is absorbed from the diet is delivered by (C) the blood to (D) the kidneys, where it is excreted via a combination of glomerular filtration and proximal tubular secretion. The increased delivery of oxalate to the kidneys leads to (E) increased urinary oxalate excretion, which in turn places these patients at risk of calcium oxalate kidney stones, corticomedullary nephrocalcinosis, and oxalate nephropathy.”
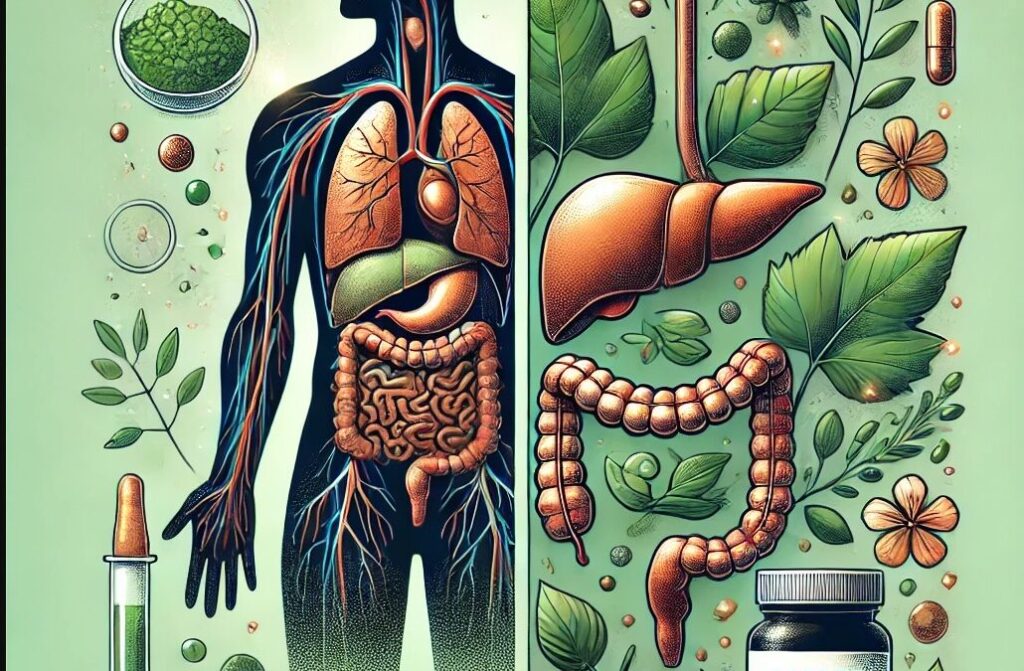
Treating enteric hyperoxaluria
There are no documented specific treatments for enteric hyperoxaluria. Current management includes reducing fat malabsorption or improving fat emulsification by improving synthesis and utilization of bile acids with bile acids, plant based cholagogues/choleretics or bile acid sequestrants. These include therapies such as taurine or glycine supplementation to support bile acid conjunction; bile acid supplementation such as ox bile; Tudca; and medicinal plants that act as cholagogues and choleretics. Plant components such as peppermint, dandelion root, artichoke, licorice, coriander, turmeric, cumin, chamomile, St. John’s Wort, rosemary have choleretic properties. Also, milk thistle is one of best studied herbal cholagogues that is known to stimulate bile acid synthesis and increase the endogenous pool of bile acids. Older studies have also demonstrated some efficacy in using bile acid sequestrants such as cholestyramine to reduce urinary oxalate excretion. This therapy has a double benefit as it can also help bind mold in the GI tract. Cholestyramine has side effects long term, so I often prefer to use fibers such as Glucomannan and Propolmannan instead. Both of these also have the secondary benefit of being able to bind and help excrete various mold species in the gut.
Integrative Therapies
Other therapies include reducing dietary consumption of fat or oxalate, using calcium supplements to bind oxalate in the gut, and increasing daily fluid intake to reduce calcium oxalate concentration. Other treatments include probiotics specific for improving microbial degradation of oxalate. In patient with Celiac or non-celiac gluten sensitivity, treatment with a gluten free diet lowers stone incidence compared to control levels. Pancreatic enzyme therapy is supportive with patients with secondary pancreatic insufficiency to reduce steatorrhea or fatty stools.
A low oxalate diet has been shown to reduce urinary oxalate excretion. A low-fat, low-oxalate, moderate-protein, and normal-calcium diet has been demonstrated to reduce calcium oxalate supersaturation in enteric hyperoxaluria. Unfortunately, this diet can be difficult for patients to maintain and may have a minimal effect on urinary oxalate excretion. Since urinary oxalate excretion in enteric hyperoxaluria correlates directly with the fat intake of the stool, it makes sense that limiting fat intake has been show to reduce urinary oxalate. A low-fat diet also improves steatorrhea, leading to less fecal fluid loss, which reduces the risk of stone formation.
Calcium supplements have been used to bind oxalates in the gut and promote excretion in the stool. I generally run Hair tissue mineral analysis to identify if there is a calcium shell first, because the excess calcium will not be absorbed and will continue to deposit in the soft tissue. So it is imperative to break down that calcium shell first before supplementing with high doses of calcium. Some practitioners like to use calcium citrate, but there are other issues with this form as most companies source this from mold or fungus. This can be a problem since another source of oxalate itself is from mold (which I will discuss in another blog).
Finally, I should mention, there are some trials going on with an oral preparation of oxalate decarboxylase as a newer potential treatment strategy. A phase 2, open-label trial in 16 participants with idiopathic and enteric hyperoxaluria found that oral oxalate decarboxylase taken for 4 days decreased urinary oxalate excretion by 14 mg/d, with a greater reduction observed in patients with enteric (−22.0 mg/d) versus idiopathic (−10.2 mg/d) hyperoxaluria. Future research may identify methods to manipulate oxalate transport in the colon and small intestine, but much work remains to better understand these pathways.
Mechanism of intestinal oxalate transport
Over the last 20 years, major progress has been made regarding the molecular identification of oxalate transporters. Several investigators have confirmed the SLC26A6 protein can actively secrete oxalate at the apical membrane of enterocytes, and loss of SLC26A6 results in hyperoxaluria and oxalate nephrolithiasis. SLC26A6 is an angiotensin activated signaling pathway, bicarbonate transport, cellular response to fructose stimulus, oxalate transport and sulfate transport.
Similar to SLC26A6, studies also indicate SLC26A1 can mediate oxalate transport.
I went back and looked at the Bob Miller software, and identified that these transporters are actually sulfate transporters. BINGO! There is a big link to sulfur and oxalates. I will discuss this in more detail in a future blog.


In summary, the belief that only going low oxalate with your diet alone is going to heal your body is a fallacy. This is why I like to do a thorough investigation of my patients that includes various lab testing. These include (but are not limited to)
Nutreval
Hair tissue mineral analysis
Mycotoxin testing
Glyphosate testing
Tree of Life Genetics
Iodine testing
Food sensitivity testing
Gut microbiome testing
Running appropriate tests short cuts the process and allows us to target interventions specific for you.
To learn more about the Root Cause investigation , please visit ICHealer.com
Learn more here
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]